eHealth NSW, in partnership with the Agency for Clinical Innovation (ACI) is supporting NSW Local Health Districts (LHDs) and Speciality Health Networks (SHNs) to rollout the Remote Patient Monitoring (RPM) Program. This Program is supporting patients with type 2 diabetes, type 2 diabetes with chronic heart failure and chronic obstructive pulmonary disease (COPD).
The Challenge
Diabetes is the epidemic of the 21st century and one of the biggest challenges confronting Australia’s health system.[1]
The total annual cost impact of diabetes in Australia is estimated at $17.6 billion (inflation adjusted).[2] Diabetes is the seventh most common cause of death by disease in Australia.[3]
Aboriginal and Torres Strait Islander Australians are three times more likely to develop type 2 diabetes and four times as likely to die from it than non-Indigenous Australians.[3]
People in regional NSW have poorer health outcomes and face significant challenges in accessing healthcare than those living in metropolitan areas.[3]
The RPM Program supports the NSW Regional Health Strategic Plan 2022-2032 by improving access to care, especially for people living in regional, rural and remote areas of New South Wales.
The RPM Program also aligns to the NSW Virtual Care Strategy, which focuses on patient centred care and equity.
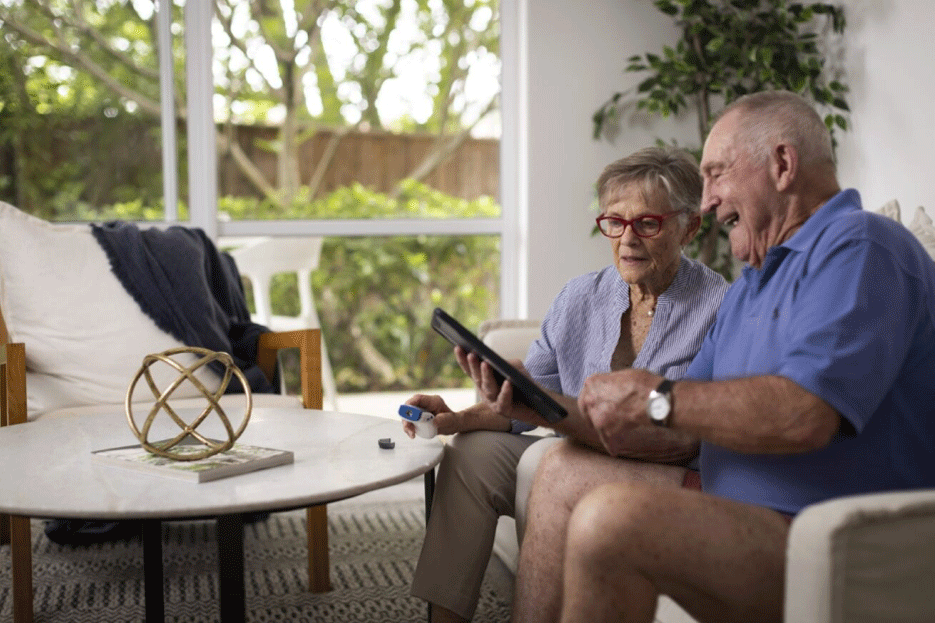
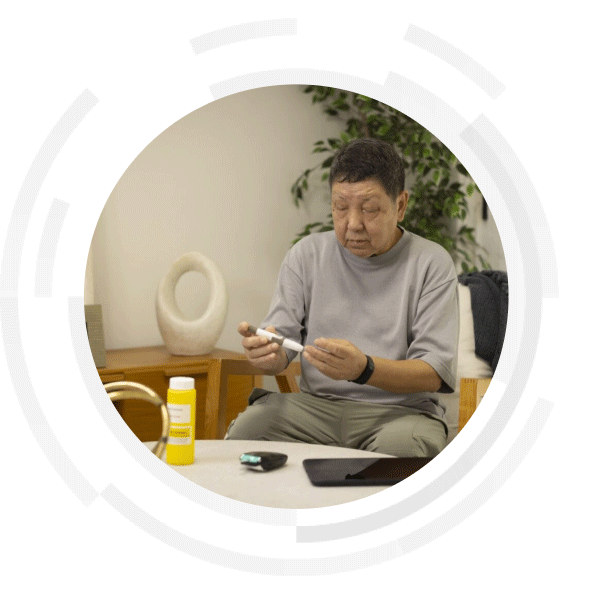
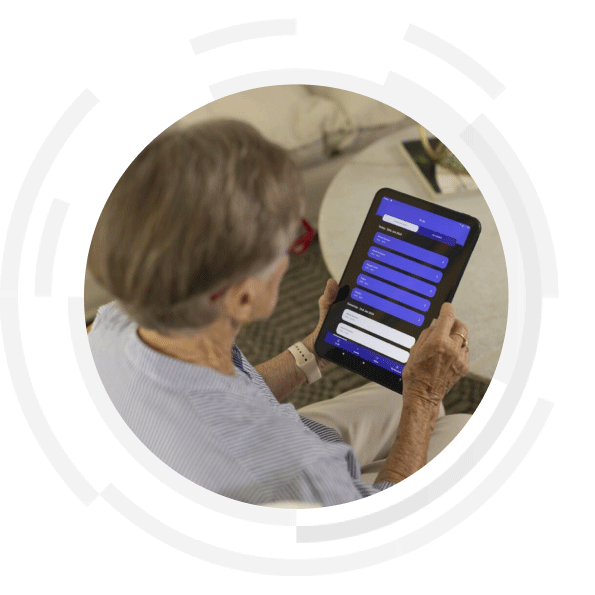
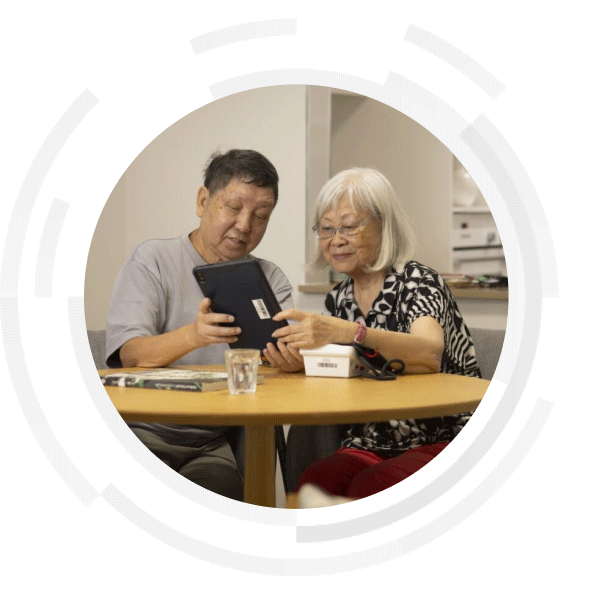
The RPM program will allow patients to receive care conveniently and safely in the comfort of their home, work, on Country or in community settings.
This program aims to reduce pressures on the hospital system through a reduction in hospital admissions, presentations to emergency department and wait and travel time for patients.
The Plan
The RPM Program supports the delivery of clinical care virtually. Patients receive a personalised kit, that may include Bluetooth biometric devices such as an easy-to-use smart tablet, infrared thermometer, blood glucose monitor, pulse oximeter, blood pressure monitor and weight scales. The devices track vital signs and allows patients to record their symptoms. This data is received by healthcare professionals who can use this information to monitor patients virtually. They receive automated alerts if a patient’s condition deteriorates enabling them to quickly intervene.
In addition to caring for patients virtually, healthcare teams can support patients and carers to self-measure and grow their understanding on how to best manage their health from the comfort of their home.
The RPM Program may be expanded in future to include patients living with other conditions.
“Remote monitoring is very worthwhile for patients who are anxious and frees up a hospital bed for someone who is really sick.” - Edna, patient in Western NSW Local Health District
The Benefits
The RPM Program provides a range of benefits for services, healthcare professionals, patients and their families, including carers.
Services will benefit from:
- reduced Emergency Department (ED) presentations
- reduced hospital admissions
- decreased lengths of stay
- improved safety and quality of care
- better integrated models of care.
Healthcare professionals will benefit from:
- enhanced clinical support
- timely access to specialist clinical advice and care coordination for both patients and clinicians
- early detection and timely intervention to avoid deterioration through virtual support
- a digitally capable workforce
- an opportunity to retain workforce and support professional development resulting from increased flexibility and efficiency, reduced unnecessary travel time, and improved clinical networks and collaboration.
Patients, carers and families will benefit from:
- care provided close to home, avoiding unnecessary transfers and delays and helping patients remain with their families or carers
- more coordinated, equitable and timely access to care
- Aboriginal and Torres Strait Islander patients can receive care on Country.
[1]Diabetes Australia. Facts about diabetes in Australia. Last accessed April 2023.
[2] Lee CM, Colagiuri R, Magliano DJ, Cameron AJ, Shaw J, Zimmet P, Colagiuri S. The cost of diabetes in adults in Australia. Diabetes Res Clin Pract. 2013 Mar;99(3):385-90. doi: 10.1016/j.diabres.2012.12.002. Epub 2013 Jan 5. PMID: 23298663.
[3]NSW Health. NSW Regional Health Strategic Plan 2022-2032.
Related solutions
myVirtualCare is NSW Health’s videoconferencing platform that provides virtual access to healthcare from anywhere i…
The NSW Telestroke Service provides patients in rural and regional NSW with 24/7 access to expert stroke clinicians…
The Critical Care Cameras and network provide clinicians with access to specialists based at different hospitals.